Multiple Disorders, One Clinician
Coordinated Program Treats Substance Use Disorder and Mental Health Issues Together
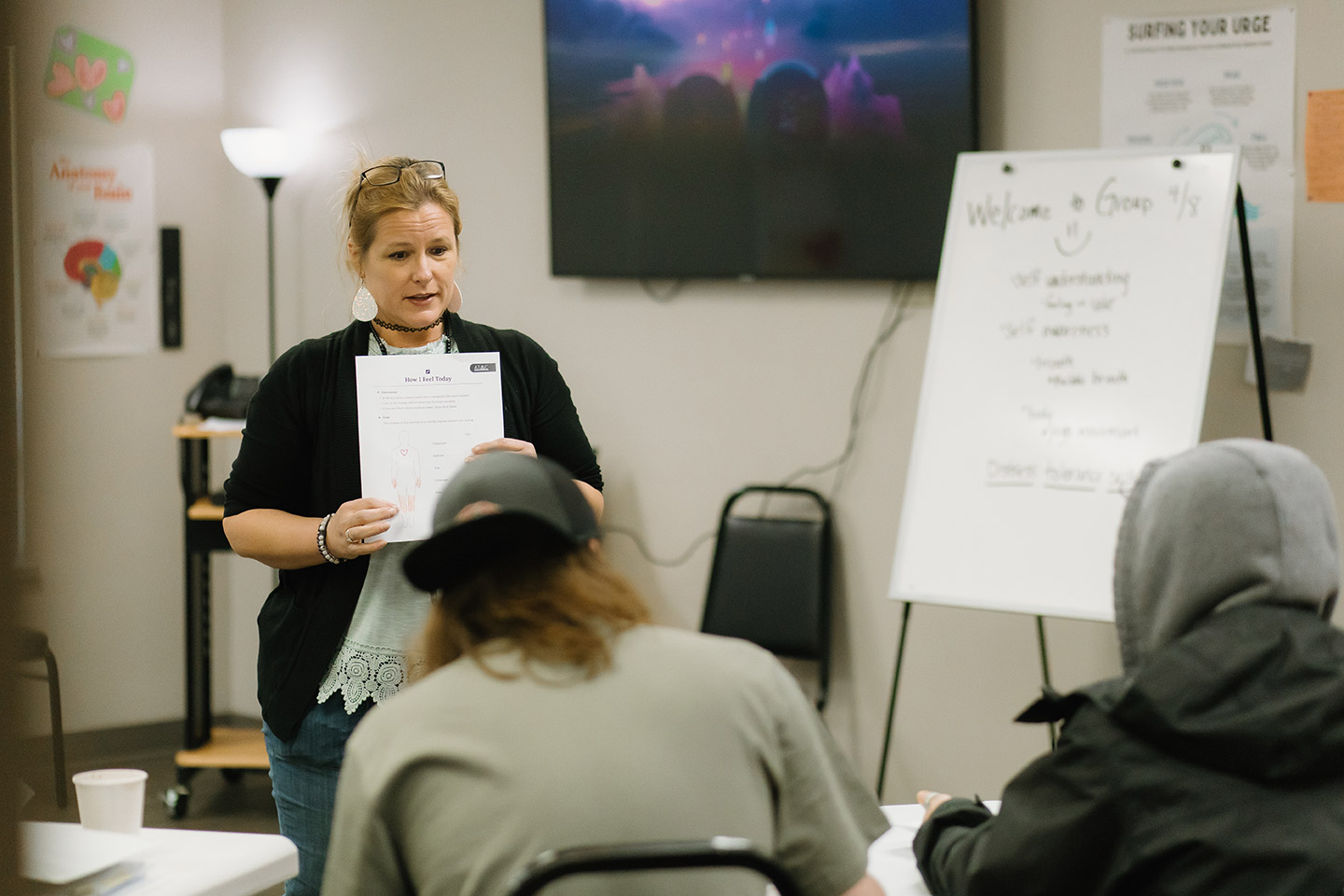
In 2024, KMHS created a Co-occurring Disorders (COD) team with clinical staff trained in both substance use and mental health disorders. The change removes a major obstacle to treatment by allowing clients to get coordinated care for both issues from one clinician.
“People with co-occurring disorders are experiencing symptoms of both mental health and substance use disorders together, so it makes sense to treat both together,” said Director of Subacute Recovery Services Wayne Swanson.
Clients can be referred directly to the program, which streamlines the process and allows them to begin treatment sooner than if they started mental health treatment and were then referred for substance use treatment.
Holistic Approach
Leann recently completed a KMHS relapse prevention class, and said the COD approach helped her learn coping skills and recognize her triggers.
“I feel that it not only helps with the drug addiction and that sort of thing, but it also helps with the mental illness part,” she said. “I can talk about what my brain is going through and what I’m feeling.”
COD Care Coordinator Rebecca Norris said many clients cope with mental health challenges by using substances. Addressing both issues at the same time provides better care and better long-term outcomes.
“We are getting to use a holistic approach, meaning addressing the medical, the psychological and the social factors,” she said.
“Clients can learn different approaches and tools and strategies for substance use, but if we’re not addressing the mental health issues and their mental health isn’t stabilized, it’s really hard for them to stay sober.”
Clients in Control
The program also gives clients more control over their recovery. They can address one issue at a time or both, and they can alternate between the two.
Rebecca said feedback from clients is overwhelmingly positive. They don’t have to struggle to keep appointments with two different clinicians – one for their mental health and another for substance use. It’s especially helpful for clients who are going through the legal system, which has its own set of requirements as clients focus on treatment and recovery as an alternative to fines and jail.
COD Therapist Graham Pernell said the approach breaks down barriers to substance use treatment.
Clients don’t have to take an extensive substance use disorder assessment to enter the program – an intense, deeply personal history that can deter clients who aren’t sure they’re ready to commit to substance use treatment.
Pernell’s role is to help clients see that recovery is possible, and that they have resources at KMHS, in the community and within themselves.
“I think 99 percent of people living with addiction feel trapped and they truly do want to change,” he said. “So, it’s just helping them see their own hope for change and see their own resources for change.”

Sober Solutions
Co-Occurring Disorder Program Helps Client Learn Coping Skills
Leann was clean and sober for eight years when her grandmother’s death dealt a blow that briefly sent her back to using crystal meth and back to Kitsap Mental Health Services for treatment.
She talked to a therapist who helped her realize it’s okay to ask for support. And that’s exactly what she did about 18 months later when she feared she might relapse.
She completed a relapse prevention course through the agency’s new Co-occurring Disorders program, which coordinates treatment of mental health and substance use challenges.
“I’m significant, and that’s what they teach me here is that I am significant. And I don’t need to use and I don’t need to take myself out,” Leann said.
Participating in the relapse prevention group has reinforced that message. “Sometimes when you’re trying to help someone else with your experience, it helps you. If I’m telling this person that they are valuable and they are worthy of sobriety and they’re worthy of all good things, then why wouldn’t that be true about myself?”
Leann’s therapist helped her move out of a shelter, off a waiting list and into a KMHS group home, where she lives with three other women who are also working on their sobriety. She’s learned new coping skills, including conflict resolution, and she’s become active in Clubhouse, a KMHS program that connects people living with mental illness and substance use disorders with a supportive community.
All of these experiences have given her a new perspective. When she’s struggling with negative self-talk, she knows to ask herself why she’s feeling that way, and to draw on tools like journaling and meditation.
“My worst day clean could never compare to a day in active addiction. Addiction means homelessness, isolation and battling the demons in my mind,” she said.
“Even though I have the battle often, I also have the coping skills and tools to not use (drugs). I have these really cool solutions, right?”
Powering Change
Therapist Motivates Clients to Find Their Strengths
Co-occurring Disorder Therapist Graham Pernell remembers the exact moment when he decided to work with people who have substance use disorders.
He was at Fred Meyer and saw a former high school classmate scouring the parking lot for loose receipts so he could get cash by “returning” items he hadn’t purchased.
“I think he had a lot of concussions,” Graham said of the former football player. “And so right about 18, 19, I could see it catching up with him. He was very impulsive. He was angry. And he turned to opioids and meth.”
When Graham saw him in the parking lot, the young man had shrunk from a muscular 240 pounds to about 150. “I said, ‘What are you doing?’ and he said, ‘I’m up to no good, man.’
“And it was kind of like a switch turned on for me where I realized that he doesn’t see any hope for himself. And, I just kind of realized that I wanted to work in the addiction field.”
That moment also prompted Graham to do some soul searching about his own substance use. He’d struggled with alcohol and marijuana, partying in high school and even picking up a DUI while earning a bachelor’s degree in Communications at the University of Hawaii.
“I really took a look at myself, and right about that point, I decided I needed to cut this stuff out if I was going to do the counseling thing for real.”
That experience now informs his work with clients. He completed a certificate program at Olympic College and went on to earn his master’s degree in 2024 from Capella University. He worked in residential and outpatient substance use treatment at KMHS before joining the co-occurring disorder team.
“It’s challenging work. It’s solving complex issues that come with mental health and substance use disorders. And it’s individual to each person I work with,” he said.
“Every client has a unique set of strengths and challenges. I think my favorite part about the job is finding out what a client’s strengths are and really leaning into those. A lot of times they’ll come in and they’ll just be so beaten down by the amount of failure that they’ve had, and I hold them accountable to the fact that they do have the power to change things.”