Community Crisis Support
Over the next 11 months, KMHS’s Mobile Crisis Outreach Team will respond to a series of crisis calls for the youngster, working with multiple state and local agencies to ensure a correct mental health diagnosis, reconnect the child to a biological parent, get the family into housing, and connect the family to intensive outpatient support through WISe.
It’s like a game of Tetris, but the stakes are infinitely higher
“We put the pieces together to make sure the child is safe,” says Mobile Crisis Outreach Manager Jenna Vyhlidal.
A Team Approach
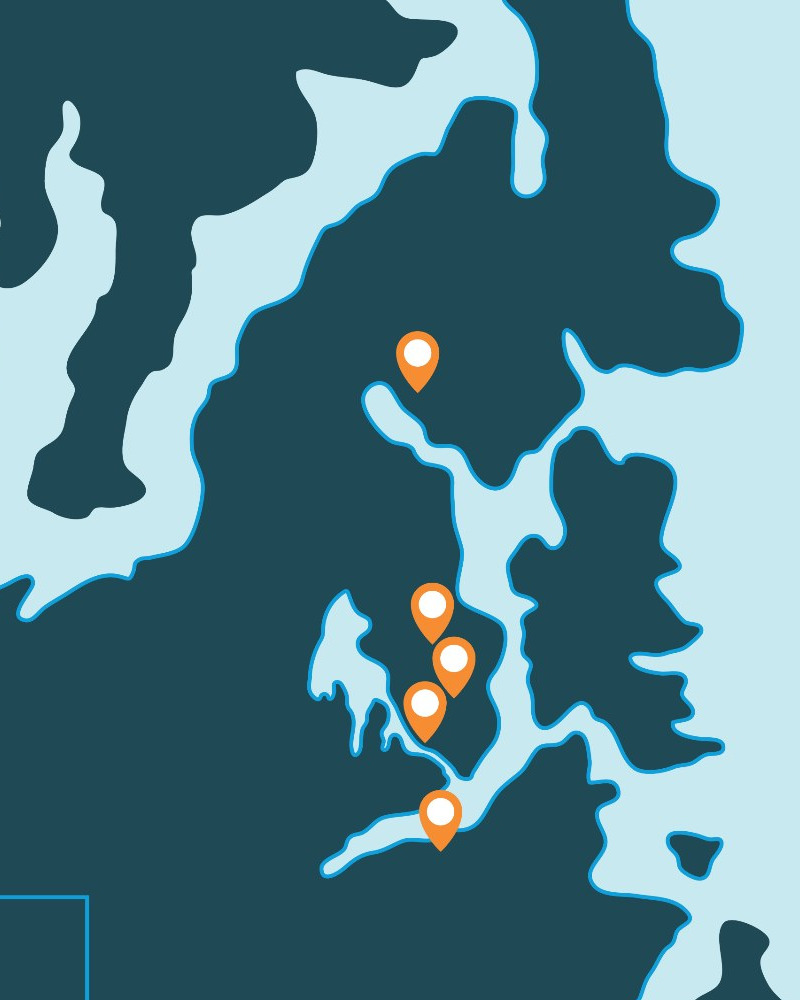
The agency created its first Mobile Crisis Outreach Team (MCOT) in 2022 and added a youth-specific program in 2023, one of the first in the state and the only youth MCOT in the Salish region of Kitsap, Jefferson and Clallam counties.
Before MCOT, mental health crisis response in Washington state centered around Designated Crisis Responders (DCRs). Their job is to determine whether someone is experiencing a behavioral health or substance use disorder so severe that they are a danger to themselves or others, and need to be involuntarily detained for treatment.
Not everyone in crisis is at that level. MCOT provides an additional layer of support, focusing on de-escalation, stabilization and connecting people to resources
“The move to mobile crisis response using mental health experts and peer counselors is a recognition by the state that dispatching law enforcement might not be the best way to deal with a mental health crisis,” says Jenna, the crisis manager.
“We are behavioral health specialists. That is our main priority, while law enforcement officers work to keep the peace.”
24/7 Response
KMHS is part of a 24/7 crisis response system, that includes first responders such as police and EMS, and the Salish Regional Crisis Line. When a person calls the crisis line at 888-910-0416, mental health professionals determine the level of support they need, and may connect them with MCOT.
Within 15 minutes of an MCOT referral, a KMHS team member calls the person in crisis to determine next steps. Do they need an evaluation for involuntary treatment? Are they a candidate for a short-term stay at the agency’s Crisis Triage Center? Or do they need MCOT to meet them in the community?
“We go where the crisis is – homeless encampments, schools, homes. One team even went to a school dance,” says Jenna.
“If people feel they’re in crisis, we’re going to help them get through that. We’re going to help them feel safe for the night and we’re going to help them get referred to resources.”
“We go where the crisis is…”
Community Collaboration
To do that, MCOT collaborates with a network of Kitsap service providers, including the hospital, the county jail, law enforcement, schools, nonprofits such as Coffee Oasis, Washington Child Protective Services and more. “We collaborate with anyone and everyone on how to help a person in our community,” she says.
Stephanie Powers, a mental health professional on KMHS’s youth MCOT, says she never knows what a shift will bring.
She typically gets called when a child is acting out or is depressed. To find solutions, she coordinates with the young person, their family and their school to identify community supports. The goal is a “warm handoff” to services such as therapy or Wraparound Intensive Services (WISe).
“It’s a hard job, but I like it,” Stephanie says. “I like being able to help families by getting down to what’s really going on and finding them services.”

MCOT Team Members
- Mental Health Professional – counselor with a master’s degree or
- Mental Health Care Provider – counselor with a bachelor’s degree plus 3 years of experience and interest in earning a master’s degree and
- Certified Peer Specialist – individual trained to share their lived experience with mental health or substance use disorders; can’t respond alone